Warmth, water, mountains, family, friends … summer means fun in the sun. But, what could be more annoying than an uptick in gut symptoms – particularly gas and bloating? No one likes to feel uncomfortable in their summer clothes.
Perhaps you can relate to this: I recently went on vacation. By the end of my time away I felt pretty good in the morning, but by dinnertime bloating was making me feel (and look) like I was pregnant.
What gives? Well, a bit of alcohol and eating more of the foods I generally avoid, added up in a negative way. And even though it wasn’t excessive, it impacted my gut in a relatively short amount of time.
If this resonates with you, don’t despair. In 10 quick days, you can reverse course. More about that in a moment.
In the meantime, here’s what you can do to support your gut for the rest of the summer…
5 WAYS TO PROTECT YOUR GUT IN THE SUMMER:
→ RETHINK ALCOHOL – Summer typically equals an increase in cocktails. Get clear: How many drinks are you consuming daily. If you’re in good health, and at low risk for cancer, then alcohol in moderation is likely okay. What is moderation? A few social drinks a week. There’s no need to drink every day, afterall. Plan for them — wait for the rooftop get-together or the weekend summertime bash. And If you’re a beer drinker, switch! Beer contains gluten and can be bloating if you’re sensitive to it. Have you considered a mocktail? Take a look at my Blueberry Lime “Margarita” recipe.
→ GET YOUR SLEEP – Long, summer days with evenings out often lead to burning the candle at both ends. When your sleep suffers, so does your gut. And don’t forget, many of your summer activities affect the quality of your sleep: drinking alcohol, consuming sugar, eating foods that don’t serve you, and even travel and activity stress can all cause sleep disturbances. And, sleep disturbances and stressors suppress your immune system, making you vulnerable to infections. Get your zzzzz’s!
→ SUPPORT YOUR GUT WITH APPROPRIATE SUPPLEMENTS – Now is not the time to leave your gut-loving supplements behind. In fact, now is the time to be vigilant. If you’re indulging in alcohol, eating foods that you generally avoid, you’ll want to make sure you’re protecting your gut microbiome and gut lining as best you can. My summer go-to’s are:
→ Probiotics – support and influence the bacteria that live in your digestive tract. Use a well-rounded, multi-strain product, and since it’s summer, opt for a shelf-stable, heat-resistant probiotic like this one: my favorite summer probiotic.
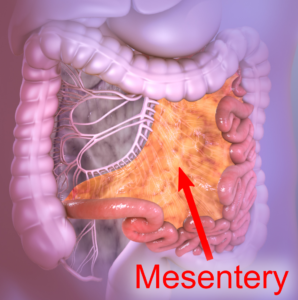
→ L-Glutamine – this important amino acid will help support the integrity your digestive tract lining by shoring tight junctions and helping to prevent a leaky gut. You want this why? Because about 80% of your immune system lives in your digestive tract and your gut lining is imperative to keeping out invaders, such as viruses (yep, like COVID). Oh, and it’s relevant to add: Alcohol consumption puts your optimal gut health at risk. Alcohol can, in fact, increase gut permeability. Here’s the the L-Glutamine I use.
→ EAT SUMMERY GUT-LOVING FOODS – Summer produce is here! Take advantage of it while you can. Make sure half of the food you eat everyday comes in the form of produce. Eat the rainbow – all the different colors offer a range of necessary phytonutrients. Plus, the fiber found in produce provides much needed food for your gut microbiome. Also consider adding some kimchi, sauerkraut and low-sugar kombucha. Some of my favorite summer foods are: berries (love them all!), herbs like basil and mint, as well as broccoli, cucumbers, snap peas, green beans, watermelon and peaches.
→ REMEMBER TO HYDRATE & REPLACE ELECTROLYTES – Hydrate, hydrate, hydrate. You might think eight glasses of water is enough. Actually, the proper amount of fluid is half your body weight in ounces. So if you weigh 150 pounds, you’re aiming to consume 75 ounces of liquid. And for every hour you’re outside, add another 16 ounces of water. Yes, really. Since it’s hot and you’re likely sweating, you might consider adding electrolytes to your day. Many of my clients like Nuun. My personal fave is Ultima.
Which brings me back to what you can do right now about summer bloating and digestive discomfort. Our 10-Day Gut Boxes will bring down the bloat and make the remainder of your summer gut-happy. Learn More Now
Happy summer!
Meet Melissa: Melissa Rapoport is the Manager of Health Coaching and Lifestyle Programming at Blum Center for Health in Rye Brook, NY. She combines her graduate work in Developmental Psychology with her education in nutrition, health and coaching to create highly individualized programs that result in lifetime change. A contributing author to three international bestselling books, Melissa’s greatest joy is her relationship with her two daughters. To learn more about Melissa’s coaching practice at Blum Center for Health, click here.


 .
.