Elimination diets are the cheapest, most effective way of identifying the foods that trigger inflammation and disease in your body. For many, elimination diets hold the key to conquering chronic pain and I use one with arthritis patients as outlined in my book Healing Arthritis.
The great news, is that elimination diets are generally short and easy to follow. My elimination diet requires just two main steps.
Step 1: Remove Gluten, Dairy, Corn, Soy, Eggs and Sugar From Your Diet For 3 Weeks
Gluten, dairy, corn, soy, and eggs represent the most common culprits for food sensitivities. Eliminating them makes it likely you’ll be cutting your problem foods from your diet. Sugar is also removed because it is a trigger for inflammation and removing it will help you learn to avoid processed foods, which usually include the common culprits, too.
A lot of times my patients ask me why we are removing all five foods at once, and whether it would be better or just as good to remove one at a time. However, first you have to remove the foods and feel better, and then you can reintroduce each food one at a time to see if you feel worse. If you only removed one food, you might not feel better because you are still eating another problem food. It would be hard to complete the experiment because you might not notice you feel worse when you reintroduce the food, because you never felt better in the first place!
Continuing the diet for three weeks will give your immune system a chance to quiet down without the food triggers around. More importantly, it should reduce your symptoms and help you feel better.
Step 2: Reintroduce Each Food One at a Time
Good job on making it three weeks without eating gluten, dairy, corn, soy, eggs and sugar! Now, you begin the second, and final, step, which is the reintroduction of each food, one at a time.
This is when you will gather all the information about whether the food is good for you or not and you’ll uncover some food sensitivities. Use this symptom chart to help you keep track.
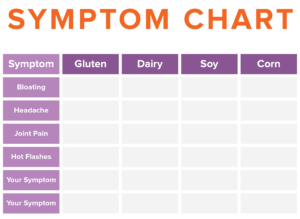
For each food that you reintroduce, think about the symptoms on your list and use none, mild, moderate, or severe to describe your reaction to it in the boxes provided. This will help you remember later when you look back.
After the three weeks on the elimination program, do the following. Introduce one food at a time: It doesn’t matter which order you choose to reintroduce the foods. I usually tell my patients to choose the food you miss most to go first. Eat that food at least twice each day, for two days, noticing how you feel. On day three, don’t eat the food, but continue to observe how you feel. If you have no reaction to the food, you are ready to move on to the next food on day four.
If you do have a reaction – such as headache, rash, brain fog, fatigue, digestive reaction, or other symptoms – stop eating it, and write it down in the above table so you don’t forget later. [Once you know a particular food isn’t good for you, remove it again.] The food reaction should go away within a day or two, but for some people it can take longer. Try the next food: Once that reaction goes away, it is time to try the next food.
Finding out if you are having a noticeable reaction to gluten is important. If you don’t have a reaction and don’t have an autoimmune disease, you can add it back into your diet. However, keep in mind that gluten is known to damage the gut, and so we still recommend eating it in limited amounts.
Be patient, because it will take you another two weeks or so to reintroduce all the foods you have eliminated. At the end of those weeks, you should now know whether gluten, dairy, corn, soy, or eggs are creating an immune reaction in your body.
Once you’ve identified your triggers you can successfully avoid them. But the better news is that it may not be permanent. Some people, after an additional period of healing, can reintroduce the foods and be symptom-free. In my own experience, I have been eating a diet 95% free of these foods for more than ten years, my reactions when I do eat them are minor compared to what they once were. They are still there, but it’s much more pleasant than it used to be!
Looking to make your elimination diet successful? Sign up for the email list (on the bottom right of this page) to stay up to date on our next article “5 Things To Know Before Starting an Elimination Diet”!