It’s been my mission to teach people how to balance and strengthen their immune systems since the release of my first book The Immune System Recovery Plan. With the emergence of Long Covid and prevalence of other viruses such as the flu and RSV, it’s more important than ever to keep your immune system in tip top shape to prevent autoimmune diseases.
It’s also essential to have an understanding of the nature of viruses and how they can impact the health of your immune system in the long run. It’s so important that I recently added an entire new chapter to The Immune System Recovery Plan that has just been re-released this month!
Viruses. Sometimes you get sick from them and sometimes you don’t.
Have you ever wondered why?
Some people can clear these viruses out of the body easily after their cold or flu, while in others the virus can persist and run amok causing problems like autoimmune disease. How does that happen?
This issue is important whether or not you have an autoimmune condition because persisting, active viruses can cause ongoing symptoms like fatigue, too. And this is something we are clearly seeing after infection with SARS-Cov2, aka “Long Covid”.
A healthy immune system should be able to respond to the infection and take care of business, clearing out the virus after a self-limited short illness. I think of a robust and well-functioning immune system as the product of good “soil” within your body.
Another name for the inner soil that grows your immune system is your terrain. Your terrain is part of a larger ecosystem that determines the functioning of, well, every system in your body.. (note the gardening metaphors).
If you have good inner terrain, you will “grow” normal functioning immune cells that can clear out the viruses. If you don’t, then they can persist. We do believe there is a genetic predisposition that allows viruses to persist and trigger autoimmunity.
But that’s not all that’s going on. Twin studies have shown us that two people with the same genetics and the same triggering virus, can have two completely different responses, all because of their terrain.
3 Viral Triggers for Autoimmune Diseases
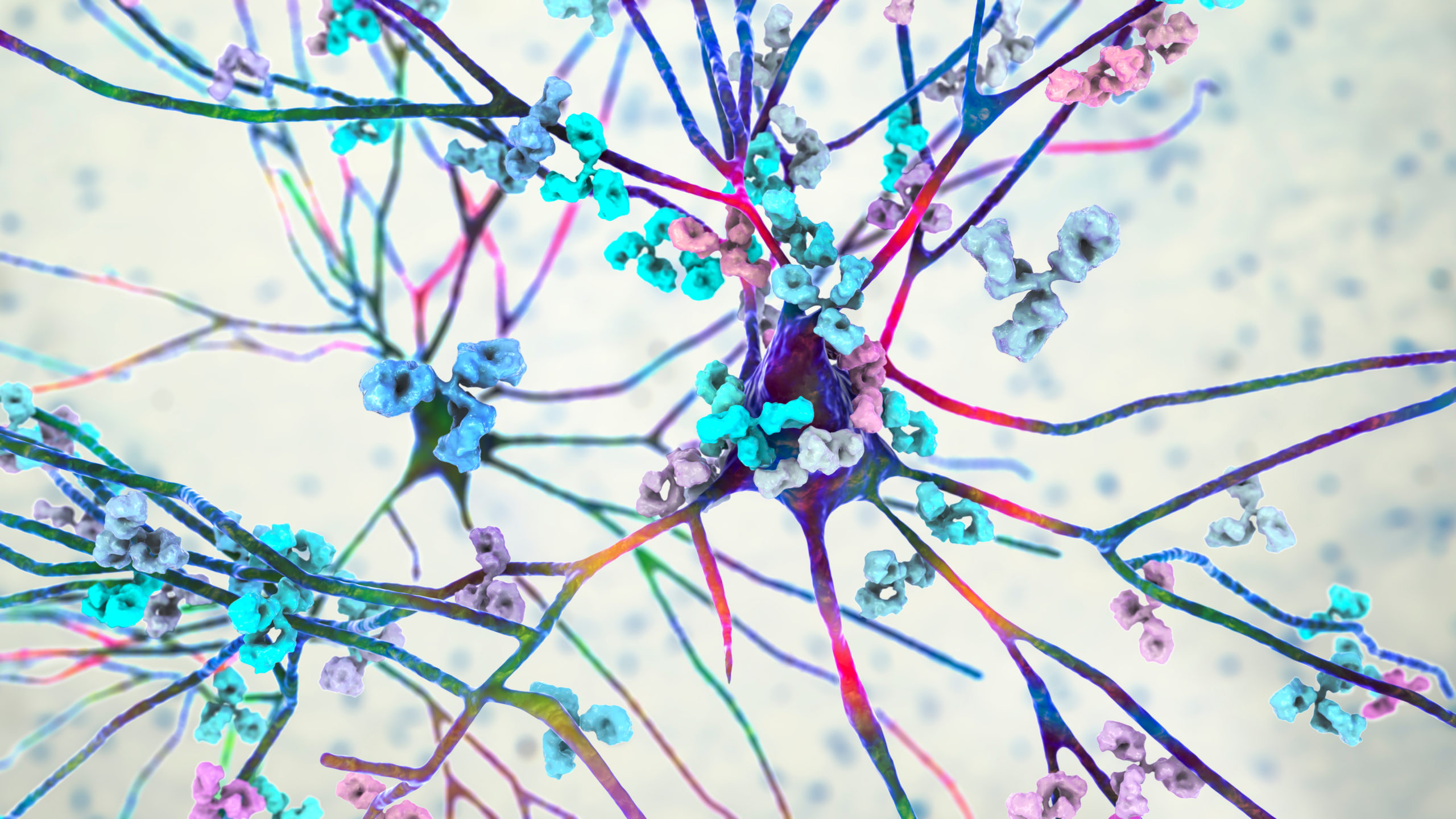
When viruses linger in the body (again, most often because of terrain issues), it is called “chronic persistence.” This leads to an ongoing antiviral immune response, which can trigger autoimmunity in a few ways.
- Molecular Mimicry: As the virus continues to spread its “proteins” around your body, there is mistaken identity as these proteins can look like your own tissue. We call this molecular mimicry. This can be because the immune response becomes less specific and it spreads to other tissues. The tissue being attacked determines which autoimmune disease you have. For example, if this happens to the myelin in your brain, then you get MS; if it’s your thyroid, then you get Hashimoto’s thyroiditis or Graves’ disease.
- Bystander Effect: Autoimmunity can also happen when the virus infects the cells directly, living inside them and causing direct cell and tissue damage. There are two things that can happen as a result, both of them bad.
The first is that your immune system reacts to the virus living inside the tissue and your body gets damaged in the crossfire. This is called a bystander effect.
The second is that the infection inside your cell causes the cell to develop a different “name tag” on the outside of its cell surface. As a result, the immune system begins to see your own tissue as foreign. If the infection becomes a chronic situation, the immune system will continue attacking your cells because the infection is still inside. An infection can persist anywhere, including but not limited to your joints, brain, and thyroid. It is even possible for an infection to live inside your immune cells themselves, which can cause your immune cells to lose their tolerance for your own tissue. Epstein Barr Virus is a good example of a virus that wreaks havoc via its bystander effect, and by persisting inside your immune cells. - Cell Damage: The final way that infections can exacerbate autoimmune conditions is when your tissues are already damaged from an autoimmune disease and then a virus is drawn to the inflammation and takes up residence in this tissue as a secondary problem. In studies that find viruses at the site of autoimmune damage, it is unclear whether the damage came first or if it was caused by the virus. Why do some people recover from an infection, whereas other peo-ple don’t? There is some evidence that in certain people bad genetics or damage from an environmental toxin or exposure has made their immune systems unable to get rid of a chronic infection. As a result, the infection triggers autoimmunity either right when the person first gets sick or because the infection persists.
I go into more detail on viruses and autoimmunity, including information about the role of specific viruses in specific autoimmune conditions in the re-release of my best-selling book, The Immune System Recovery Plan. I’ve added a whole chapter dedicated to this very topic.
But you can see, no matter the mechanism, to prevent and treat autoimmunity that has been triggered by viruses, you want to make sure your immune terrain is functioning well so that the viruses are cleared out and not allowed to become chronic persisters.
Here is how to improve your terrain to create a robust and healthy immune system to clear out viruses:
Nutrition:
Eat an Anti-inflammatory Diet: whole foods rich in antioxidants and fiber, low in sugar, animal and processed fats; elimination of foods that trigger inflammation including gluten and genetically-modified foods. Overall, eat less food from animals and more from plants. Remember to focus on eating more of the GOOD foods, not just on eliminating the bad.
Supplements:
I’ve put together my favorite supplements that include vitamins, minerals and antioxidants that your immune system needs for optimal well being.
Balanced Hormones:
-
- Make sure your stress system and adrenals are balanced and resilient. To do this, you must focus on your lifestyle, which includes sleep, exercise, daily relaxation, reducing toxins in your food and environment, and eating nourishing food. The good news? These are things all of which you have control over!
- Sex hormones: No matter where you are in your life, we all have hormones that we need to help our bones, muscles, life force and immune system. As we age, sex hormone levels are tied into stress.
Join our meditation classes and learn how to destress, relax and as a result improve the functioning of your immune system and hormones.
Healthy Gut:
-
- Daily goal should be to support your Intestinal ecosystem. A “good gut” means that you have adequate beneficial bacteria, good barrier function (no leaky gut), and no “weeds” in the inner garden.
- Digestion: a healthy gut also has good stomach acid, bile acids, and pancreatic enzymes so that you are digesting and absorbing all the nutrients from the food you eat.
Sometimes, the gut microbiome just needs a good “reboot” to clean out the bad bacteria and yeast that can grow as a result of stress, illness, antibiotics or other medication, poor food choices, to name a few. Our Gut Cleanse Box was designed to help you easily treat your microbiome which can improve digestive symptoms, reduce inflammation, reduce food sensitivities, improve memory and mood, and even help you reach your ideal weight. The packets are filled with herbal antibiotics (pills) that clean out the bad bacteria and yeast. If you would like to be guided by a wellness coach while you do your gut cleanse, check out our HealMyGut Programs.
Well Functioning Liver:
-
- Daily goal should be to reduce your toxin exposure and eat foods that support your liver’s detox system so that you can maintain a low toxin load in your body. Toxins damage the immune system. It’s often the total amount of all toxins that make you sick, not just one in particular.
- Clean up your environment and make sure your “biotransformation pathways” through your liver are working well
- This will also support your Estrogen detox pathways, something that everyone needs to pay attention to, because toxic estrogens can cause damage in the body.
It’s important to detox your liver safely and effectively. I’ve put together a Detox Repair Kit that will renew your body and reset your system by eliminating your toxic load.
Remember, you can’t avoid viruses! They are everywhere. Instead we work on creating resilience in the immune system so that the viruses don’t become chronic. To do this, we focus on the terrain of the immune system, which leads to the 4-step Immune System Recovery Plan, the focus of my first book on autoimmunity being re-released this month. Grab your copy here.
References:
Vieira et al. Diet, microbiotia, and autoimmune diseases. Lupus 2014 23: 518
Getts, D, et al. Virus, infection, antiviral immunity, and autoimmunity. Immunol Rev. 2013 September; 224 (1): 197-209.
Vanderlugt, C, and Miller, S. Epitope spreading in immune-mediated diseases: implications for immunotherapy. Nature Reviews Immunology 2, 85–95 (1 February 2002)